1. Bring Mindfulness Into Your Day Stress and anxiety don’t just affect your mind—they impact your nervous system, sleep, recovery, and even how your body experiences pain. Mindfulness and meditation,
Physical Therapy for the Elderly
February 26, 2021 3:24 pm / Category: Physical Therapy
Many people misconstrue physical therapy as beneficial only for folks recovering from injury or illness, athletes, or a specific demographic. The truth is that physical therapy can benefit anyone of any age or fitness level. Here is an insightful look into how it can foster maximum function in the elderly.
Physical therapy has an important role in health care delivery and is connected with maximizing function, preventing decline, decreasing pain, and treating physical illnesses. For elderly individuals, who often have decreased physical reserve, any medical illness can lead to decline. Inactivity and bedrest, a common consequence of illness, contributes to and intensifies muscle weakness, causing deterioration in walking and loss of function. Illnesses, such as Parkinson’s disease, fracture, or stroke, can affect walking and balance directly. Chronic diseases, such as arthritis, may cause pain or restriction of movement. Exercise, activity, and other physical therapy interventions can therefore have a profound effect on overall health, restoring an individual’s ability to perform the daily activities required to live independently in the community.
Assessment
Evaluation begins with a patient interview to determine the individual’s perception of the problems and their goals for treatment and then proceeds to a physical exam. Typically, a physical therapist will assess a wide array of abilities, including strength, balance, transfers (rise from a chair), and walk.
Assessment of muscle strength, through manual muscle testing, can determine whether the strength of a particular muscle, graded from five (normal) down to zero (completely dysfunctional). Muscle weakness is commonly associated with problems walking and climbing stairs, as well as falls. Appreciating the relationship between strength and function can clarify the expected degree of difficulty an individual will have with daily tasks. Other areas evaluated include sensation, range of movement, coordination, and muscle tone (i.e., a measure of the ability to relax when an extremity is passively moved).
Pain is another common problem that limits abilities. If pain is present, it is important to determine the duration of pain, describe what exacerbates and relieves the pain, get an indication of severity, and formulate a comprehensive treatment plan for pain control.
The impaired balance will affect the ability to walk safely and can contribute to falling. By observing an individual in the sitting or standing position, static balance can be determined. Dynamic balance, or balance during movement, can be assessed by watching an individual’s ability to react to perturbation and displacement.
Physical therapists will judge walking safety, evaluate gait patterns and posture, and appraise a person’s ability to transfer safely from a bed or chair to a standing position. Transfer and gait can be described by the amount of assistance that is needed to safely accomplish these tasks and can be grossly classified as independent needing assistance (of one or more people), or unable. A specific gait pattern may point to a medical diagnosis, such as Parkinson’s disease, stroke, or uncontrolled pain.
Sometimes home safety assessments can delineate problems in the environment that predispose the patient to fall. Common problems include scattering rugs, poorly lit areas, low chairs, and clutter.
Assessment tools are frequently used to standardize evaluation and measure treatment outcomes. These tools allow the physical therapist to record and communicate information in a consistent fashion. For example, both the Berg Balance Scale (scored from 0–56 with 56 being the optimal score) and Functional Reach Test (ability to reach forward, calculated in inches) measure balance. Mobility scales include the Elderly Mobility Scale (scores a person’s ability to transfer, stand, reach, and walk) Timed Up and Go (amount of time required for a person to rise from a chair, walk 3 meters, turn and return to a seated position in the chair), and a 6-Minute Walk Test (a measure of the distance a person can walk in this time). There are many activities of daily living scales (Barthel Index and Lawton Brody) that can be used to document a person’s abilities to carry out basic tasks (i.e., dressing, bathing, walking, hygiene).
Functional ability is important as it affects the quality of life, emotional status, and ability to remain independent.
Treatment
Treatment must be tailored to the physical and functional problems identified during the assessment. Muscle weakness and lack of strength can be treated with resistance exercise. An exercise technique known as high-intensity resistance training (HIRT) can be used in different clinical settings, from nursing homes to community programs. Research shows that high-intensity resistance training is safe, well-tolerated, and can increase muscle strength by as much as 113 percent. Even people who are very weak are able to tolerate and benefit from this form of exercise.
Pain control is essential to achieve optimal function and quality of life. Mechanical aspects of pain can be helped with sketching, the use of an aid or orthotic, or activity modification to achieve joint protection. Exercise can remediate pain, as is the case in osteoarthritis. Pain associated with inflammation or swelling can be treated with the use of modalities such as ice, heat, transcutaneous electrical stimulation (TENS), ultrasound, or acupuncture. Medications can be used adjunctively when necessary.
Gait and balance training is an integral part of treatment. Gait training is aimed at improving postural alignment, gait pattern, speed, safety, and endurance. A walking aid, such as a cane or walker, an orthotic, or appropriate footwear may be recommended. To help with stability, balance responses are practiced to promote appropriate reactions. Weight-shifting exercises and functional activities, such as reaching, can be helpful.
Aerobic conditioning can improve cardiovascular function and endurance and is an especially important component of a cardiac rehabilitation program.
These interventions often improve an individual’s physical condition and restore function. Sometimes, physical problems cannot be entirely alleviated, but usually, therapy can help an individual adapt to disabilities, allowing for increased independence and improved safety.
Interdisciplinary approach
The physical therapist typically works closely with other health care professionals, such as nurses, physicians, social workers, and occupational therapists, in order to refine both diagnosis and treatment. This interdisciplinary approach allows for the integration of all domains of health to more fully address the needs of the elderly.
Conclusion
For the elderly population, illness can quickly affect physical stability and cause deterioration in walking. Alternatively, a decline in physical function can cause deterioration in health and quality of life. Therefore, physical therapy interventions are an essential aspect of health care delivery. Exercise and other therapeutic treatments provide options to address inactivity, muscle weakness, and specific physical and medical problems. Using these techniques, the physical therapist is able to improve function, optimize safety, and ameliorate painful or dysfunctional conditions.
Reference: {https://www.encyclopedia.com/education/encyclopedias-almanacs-transcripts-and-maps/physical-therapy-elderly}
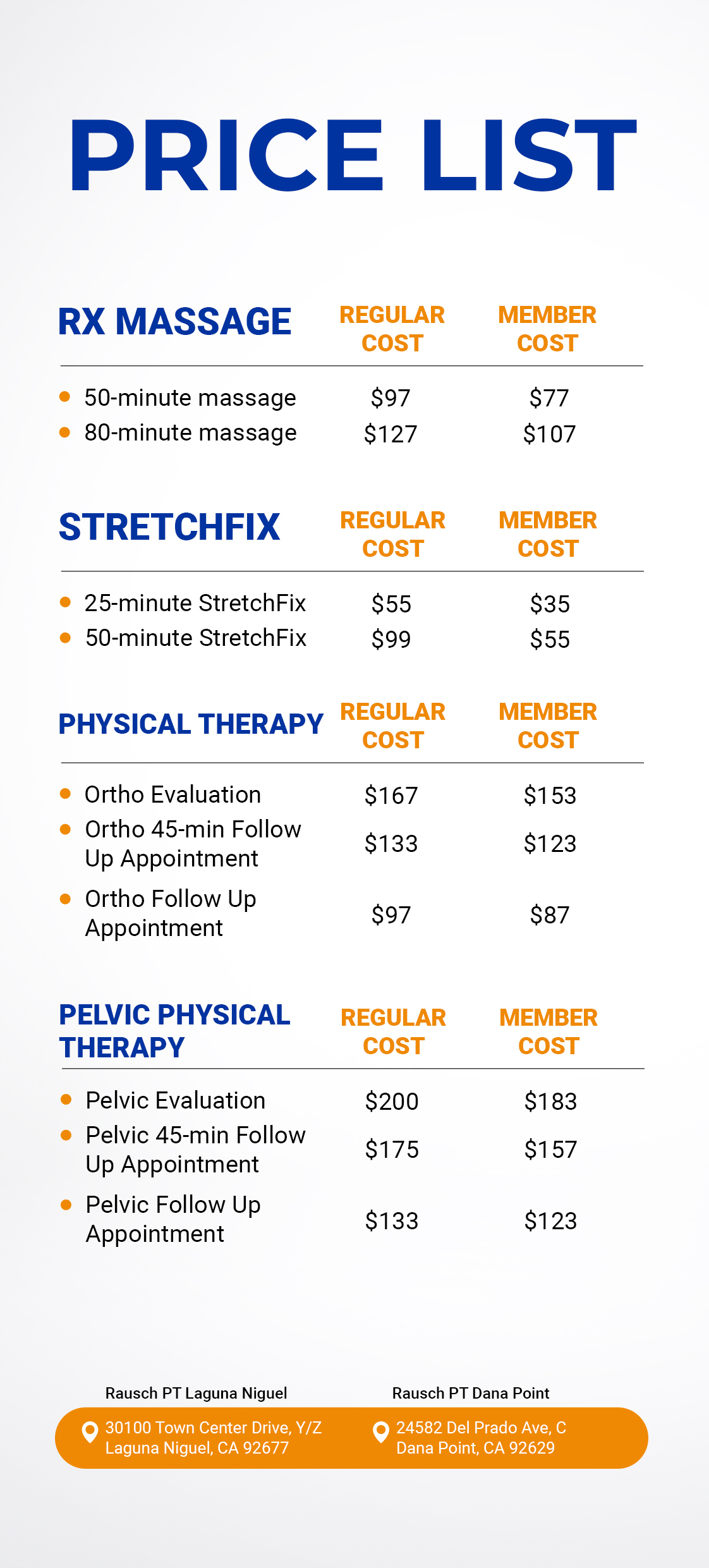
Rausch Physical Therapy remains your caring team and can accommodate you with a specific, personalized plan. Visit our Facebook page at https://www.facebook.com/rauschpt or call us at (949) 276-5401 to learn how we can help you. Don’t forget: there’s no prescription needed to see a PT in California.
Let’s talk! We are here to help. Give us a call for a complimentary consultation. We would love to meet you.
Did you know there’s no prescription needed from a doctor to see us – but we will communicate your progress and treatment to your doctor if you’d like us too! (949) 276-5401
Disclaimer — All the information that you find on our blogs and social media pages is for informational purposes only and is not intended to be used as your personal professional diagnosis, or treatment. Come and see us for your excellent, personalized care! https://rauschpt.net/