1. Bring Mindfulness Into Your Day Stress and anxiety don’t just affect your mind—they impact your nervous system, sleep, recovery, and even how your body experiences pain. Mindfulness and meditation,
Anthem Blue Cross To Limit Members’ PT Starting November 1
June 2, 2024 6:00 am / Category: Uncategorized
Are You a Patient with Anthem Blue Cross?
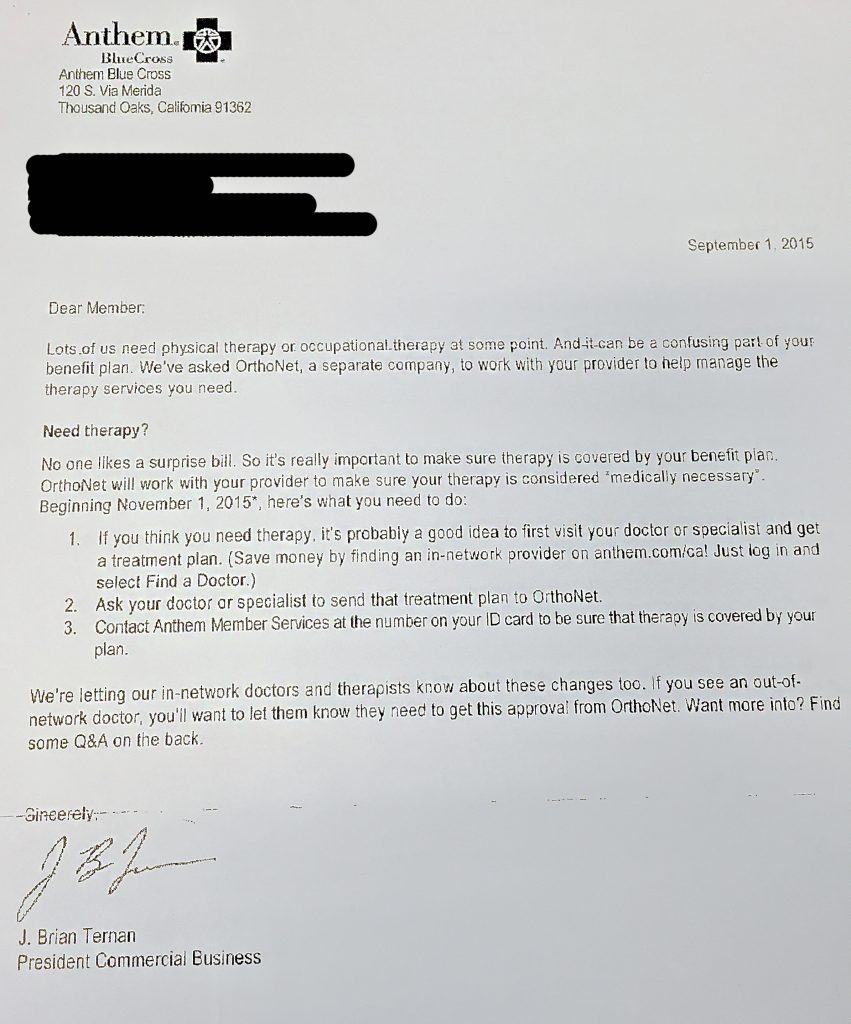
Do you use Anthem Blue Cross as your primary health insurance company? Have you received this letter in the mail?
Confused? Angry? You should be! Essentially, the people you pay so you can have access to medical care are telling you they’re going to start limiting your access to medical care. By hiring a third-party to decide if your physical therapy treatment is “medically necessary” (a legal term, not a medical one), Anthem Blue Cross (BC) is opening up new channels for being able to avoid paying for your medical care.
At Rausch Physical Therapy, we work hard to provide exceptional, quality care that is easily and affordably accessible, and it’s troubling that this practice of limiting your access to medical care has become the norm for medical care insurance companies.
How Rausch PT currently handles insurance companies/payment
Regardless of what that letter above implies, since the passage of the Direct Access bill in 2014 Californians have not needed a doctor’s referral/prescription before coming into a physical therapy clinic for treatment. You can come to Rausch Physical Therapy at any time for any injuries or impairments that prohibit your mobility, function, and/or quality of life. The issues only arise when it comes to figuring out who pays for this treatment.
Ever since it opened in 2006, Rausch PT has been on the leading edge of forward-thinking healthcare, and Direct Access made possible what owner Kevin Rausch had always envisioned: all people having an easy entry point onto the road to rehabilitation and recovery.
Currently, once our patients come in our door they have two options to pay for their medical treatment:
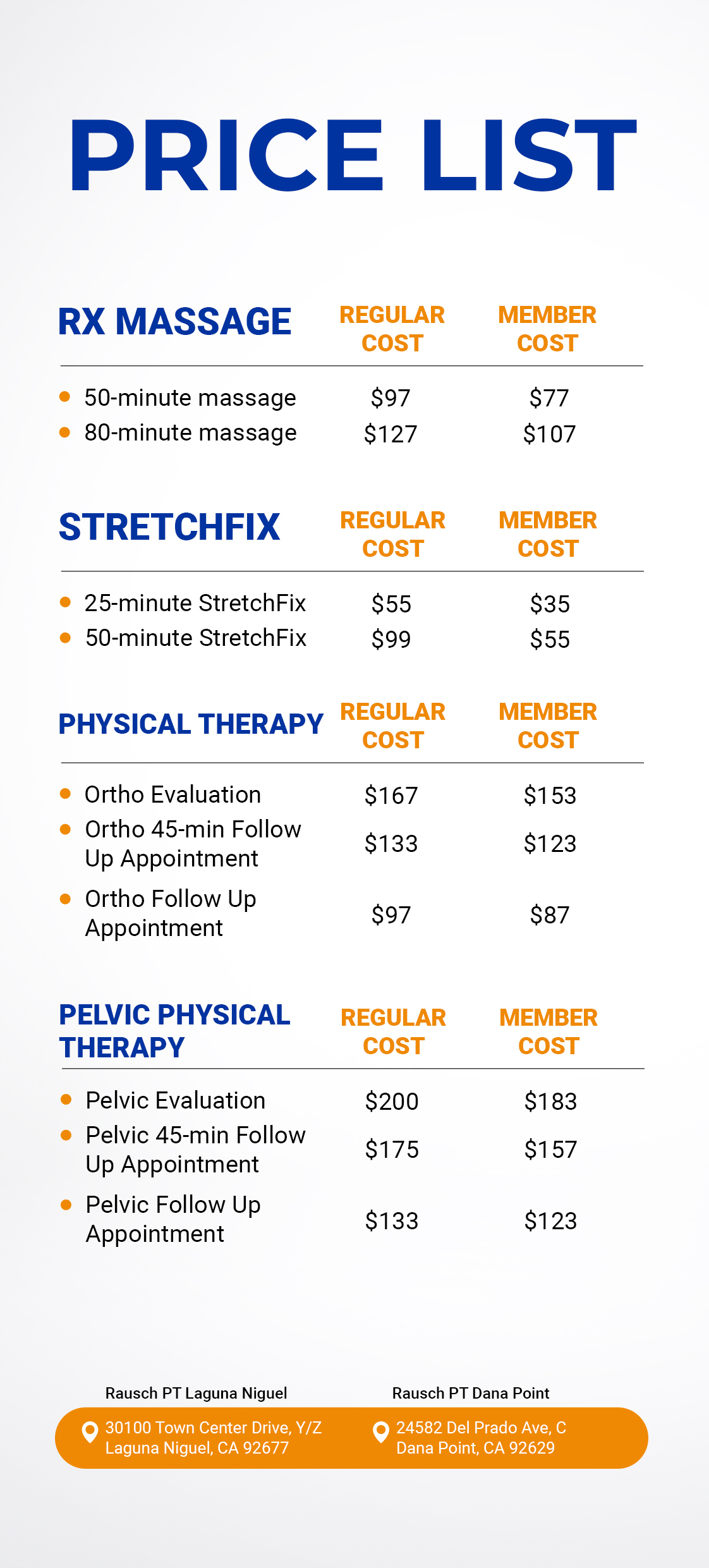
- Pay an out-of-pocket cash rate
- Have their insurance help cover the cost of their visit; once we submit their claim to and receive approval from their insurance company, the patient is only responsible for their copayment or deductible.
Whichever payment option you choose, everyone from our front office staff to your physical therapist to our billing department is dedicated to providing you with the best experience and highest quality of care possible.
How the introduction of OrthoNet affects you
Following the lead of other large health insurance companies, BC has decided to bring in a third-party management company, in this case OrthoNet, to handle the authorization of its physical therapy treatment claims. It’s OrthoNet’s job to scrutinize every claim request we submit on behalf of a patient to determine if said visit is—by OrthoNet’s definition—”medically necessary.” After we submit your claim, OrthoNet has two business days to gather all the necessary “clinical information” and either approve or deny your request. If they do approve your claim, OrthoNet will then tell you exactly how many visits it should take you to get better in and subsequently will only pay for.
Please note that this change does not affect BlueCard or Blue Cross Blue Shield members.
Why is this troublesome?
Let’s use the curious cases of Jenny and John as examples to illustrate the potential pitfalls of this increasingly-popular decision by medical care insurance companies to hire third parties to manage their physical therapy claims.
Jenny’s Case
What happens if your claim is denied?
[toggle title=”Click to read…”]Jenny loves to run, but she pushed herself a little too hard this triathlon season and now has knee pain that’s started to limit her ability to train. As an Anthem Blue Cross member, Jenny decides to take advantage of those 60 physical therapy visits she’s allotted per year and immediately makes an appointment at Rausch PT. During Jenny’s first appointment, the front desk sends a request to OrthoNet to get approval for payment for Jenny’s appointment. Jenny sees her PT, and after his initial, hands-on evaluation, he believes Jenny will be back to running pain-free after four or five visits.
Meanwhile, someone at OrthoNet is reviewing Jenny’s case and decides physical therapy treatment for her chronic knee injury is not medically necessary. She does not need surgery (yet) so they deny paying for treatment. They cover the cost of the initial visit, but Jenny now must decide if she’s going to pay cash rate to continue with her compelling treatment plan that will allow her to continue doing what she loves.[/toggle]
John’s Case
What happens if your claim is approved?
[toggle title=”Click to read…”]John is a senior in high school and has sprained his ankle playing basketball. John’s mom received the letter above, and per Anthem Blue Cross’ suggestion she makes an appointment for John to see an in-network doctor. Two days and $150 later, John comes in to Rausch PT with doctor’s approval in hand, ready to start getting better.
On his first visit, we send a request to OrthoNet to get approval for payment for John’s appointment. John sees his PT, and after her initial, hands-on evaluation, she tells John he should be 100% after four or five visits and back on the court before playoffs start in two months.
Meanwhile, someone at OrthoNet is reviewing John’s claim, and two days later they send a payment approval notification. However, OrthoNet has determined that John’s sprain isn’t that bad, so he should be able to start feeling better after a couple visits. BC will only help pay for two appointments to treat his ankle.
John and his PT work hard in those two visits, but he’s still only at about 60%. Inevitably, John is put in a difficult position: does he continue treatment by paying out of pocket so he can make it back in time for playoffs, or does he stop treatment and retire his jersey—or worse yet, try to play anyways and potentially cause lasting damage?[/toggle]
The takeaway
It’s unfortunate that even if your physical therapist—or even your doctor—understands your treatment as medically necessary, an outside company can still refuse to acknowledge it as so and require you pay for treatment on your own (on top of you still paying for health insurance.) It’s even more frustrating to us as a provider that we can be limited in the amount of treatment we can give people who come to us for help.
Our patients have and always will be top priority at Rausch Physical Therapy; our sole concern is getting you feeling better so you can get back to doing what you love. Our team of licensed physical therapists spent many years in school to receive their bachelor, master and doctorate degrees and licenses so they could diagnoses and relieve chronic pain and heal injuries to give someone a better quality of life. We don’t believe you should have to live with pain for any reason, especially if that reason is because an outside management company says treatment for your pain isn’t “medically necessary.”
What Rausch Physical Therapy is doing to help
- During the last week of October, our front desk staff will be contacting our Anthem Blue Cross patients who are already scheduled for treatment on or after November 1. Together, we’ll work to complete the additional paperwork required to request “prior authorization” so we can continue providing you with quality treatment through the end of the year. Again, this change is effective November 1, 2015.
- At Rausch Physical Therapy, we believe that everyone should have easy, direct access to PT, a physical medicine and rehabilitation specialty that we see change lives every single day. To prepare for the potential influx of BC claim denials after November 1, we are currently working on rolling out new, innovative ways to give you, our valued patient, more payment options so you will never have to rely on referrals or allow your health insurance company to limit your health.
What can you, the patient, do to help?
- Raise a ruckus! Be proactive. Demand access to the care you pay for and deserve. Call the Anthem Blue Cross customer service number. Then email your friends, get on Facebook, Tweet, and share this.
- If your claim is denied for being “medically unnecessary… Fight back and appeal. According to the U.S. Government Accountability Office, you have a 50-50 chance of getting your appeal approved if it’s an issue of medical necessity. It may take a little longer, but if the amount of money is significant or the issue important enough to you, it is worth the time you take to make it right. Get the forms you need and fill them out and send them off. Rausch PT and/or your doctor can help by providing additional medical information to the request to show exactly why it is medically necessary. Don’t be intimidated by your insurance company; we’re here to help. Click here for the forms you need to file a complaint.
If you have any questions, please feel free to call our office at (949) 276-5401 and we’ll be happy to answer any concerns you may have to make this transition as easy as possible.